Tinnitus – Ringing in the ears
1. What is tinnitus?
Tinnitus is abnormal sounds, such as buzzing or whistling in the ears that the patient hears intermittently or all the time, in the absence of any source of sound in the surrounding environment. Affecting one ear or both, tinnitus can be simple or complex and may or may not be accompanied by deafness. Tinnitus is a veritable public health problem. According to different epidemiological studies, its prevalence is evaluated as 1% to 8% of the adult population. A study conducted on over six hundred tinnitus patients has also demonstrated that 26% suffer from a significant deterioration in their quality of life, with substantial behavioural changes: irritability, anxiety, tension and sleep depravation. The lack of success of several treatments, particularly drug therapies, has led some teams to propose therapies based on radically different concepts.
All tinnitus patients require a careful otoneurological assessment conducted by an ENT specialist to try to:
1. determine the cause
2. adapt treatment accordingly.
2. Physiopathology of tinnitus
Two hypotheses have been offered as to the cause of tinnitus: a peripheral cause and a systemic cause.
ENT
To find out more, download the document below:
3. Determining the consequences of tinnitus
Different questionnaires have been developed to determine the functional, physical and psychological consequences of tinnitus. They can also be used to assess the impact of a given treatment. There are several types. The following are most often used:
1. The Tinnitus Handicap Inventory (THI) (Newman, Jacobson and Spitzer, 1996), developed specifically in English-speaking countries to determine the debilitating effects of tinnitus (25 questions subdivided into functional, emotional and catastrophic consequences).
2. The THQ, tinnitus handicap questionnaire, is the one most often used in France.
It includes 27 questions (graded 0 to 100).
4. Audiometry
The pure tone and speech audiometry, accompanied by a tympanometry and an impedance measurement, is an essential examination. The majority of tinnitus cases are associated with auditory loss but 20 to 30% of patients can have normal hearing. Tinnitus often accompanies age-related high frequency hearing loss but also hearing loss caused by exposure to noise through the person’s occupation or leisure activities (hunting, concerts).
During this examination, the ENT specialist also tries to determine the predominant frequency of the tinnitus (tinnitus frequency test). This test helps to diagnose the cause. When the tinnitus is predominant in lower frequencies, this indicates a condition involving the secretion of endolymphatic fluids. When the tinnitus affects high frequencies, it is often associated with a unilateral scotoma (asymmetrical hearing loss on one frequency) for which the cause must be determined.
Auditory evoked potentials may also be necessary to detect a problem with the auditory nerve, such as that caused by an acoustic neurinoma. Otolithic evoked potentials induced by intense sounds can indicate a canal dehiscence when early waves (P13-N23) are asymmetrical in amplitude.
5. X-ray examination
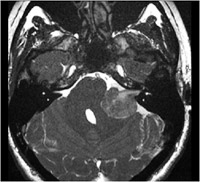
An MRI focusing on the internal ear canals must be conducted in the event of unilateral tinnitus with or without unilateral deafness, in order to detect damage to the auditory nerve. In certain cases of conductive deafness, a thin section scan of the petrous part of the temporal bone can be useful to detect otosclerosis, a traumatic impairment, or a canal dehiscence.
Blood work is necessary, including FBC, SR, lipid profile, and zinc and thyroid hormone assays. It is also essential to monitor blood pressure.
6. Treatment
Different types of treatment can be offered:
• Medical treatment
Medication used to stimulate blood flow such as trimetazidine and ginkgo bilboa (Tanakan) can be useful. Gaba agonists (neurontin) and dopamine agonists (piribedil) specifically affect the efferent auditory system. Afferent neural pathway inhibitors, such as carbamazepine (Tegretol), are also recommended as they reduce hypersensitivity of the auditory centres. Tranquilisers or antidepressants reducing serotonin reuptake may also be prescribed. Recent studies have also shown that acamprosate (an NMDA receptor blocker and Gaba agonist) has been effective in some cases.
• Relaxation techniques
Techniques used to reduce autonomic nervous system activity (sophrology, yoga) can be beneficial.
• Cognitive therapy
Cognitive behavioural therapies (CBT) have progressed considerably over recent years. They are based on a brief pragmatic approach, using optimum adaptation and coping strategies both in terms of cognitive aspects (by modifying unhelpful thought patterns) and in terms of behavioural aspects (by modifying inappropriate behaviour). The goal is to help patients who are disabled by their tinnitus to reach the state of neglect that most tinnitus patients reach spontaneously. The auditory pathways project not only to the auditory cortex but also to the limbic system, which is responsible for the patient’s state of anxiety. CBTs are also effective on anxiety or depressive conditions preceding or induced by the onset of tinnitus.
• Hearing aids
Hearing devices serve to:
1. mask the tinnitus and
2. reduce the asymmetry in hearing which is the cause of plastic changes in the auditory centres (inferior colliculus, auditory cortex), which fundamental studies have demonstrated are reversible.
It is therefore possible that in the future, a hearing device that selectively amplifies the hearing loss frequency zone could be used to treat the tinnitus without the patient having to wear the hearing aid all the time.
• Surgery
Inner or middle ear cochlear implants, magnetic and electrical stimulation of the primary or secondary auditory areas are being assessed after fMRI characterisation of the abnormally activated cortical areas..
7. Conclusion
ENT specialists are no longer at a loss to treat tinnitus patients: gone are the times when patients were told that they would have tinnitus their whole lives and that they would simply have to get used to it. The doctor should reassure the patient and offer different treatment solutions ranging from the less aggressive (drugs, cognitive behavioural therapies, hearing aid) to the more invasive (surgery). Multidisciplinary management is often useful. Lastly, progress in fundamental research has helped healthcare professionals to better understand the cause and to develop new treatments. This area is still seeing major developments.


 Bulletin numero 4
Bulletin numero 4